
shin splint stretches pdf
Understanding Shin Splints: Causes and Symptoms
Definition and Medical Explanation
Shin splints, or medial tibial stress syndrome, involve pain along the inner edge of the tibia, often due to inflammation of the bone and surrounding tissues.
Common Causes of Shin Splints
They typically result from overuse, such as repetitive running or jumping, improper footwear, or running on hard surfaces without proper warm-up.

Identifying Symptoms and Early Warning Signs
Symptoms include dull, aching pain along the shinbone, mild swelling, and tenderness to the touch, often worsening with physical activity.
Shin splints, medically referred to as medial tibial stress syndrome, are an overuse injury causing pain along the inner edge of the tibia. This condition occurs due to inflammation in the bone and surrounding muscles and tendons. While not as severe as a stress fracture, shin splints can disrupt training and daily activities. The pain typically develops gradually and is often linked to repetitive stress from running or jumping. Early diagnosis is crucial for effective treatment and recovery.
Shin splints often arise from repetitive stress on the lower legs, typically due to running, jumping, or high-impact sports. Overuse injuries, sudden changes in training intensity, and inadequate footwear are primary contributors. Running on hard surfaces, poor running mechanics, or muscle imbalances can also trigger this condition. Additionally, weak or tight calf muscles and insufficient warm-up routines may exacerbate the risk. Identifying these factors is essential for prevention and recovery.
Shin splints typically present with a dull, aching pain along the inner edge of the shinbone, often worsening during or after physical activity. Early signs may include mild tenderness or soreness that subsides with rest. As the condition progresses, pain may become sharper and more persistent, accompanied by swelling or redness in the affected area. If left unaddressed, even simple movements like walking can become uncomfortable. Recognizing these symptoms early is crucial for effective management and prevention of further injury.

Prevention Strategies for Shin Splints

Wearing proper footwear, incorporating orthotics, and gradually increasing physical activity can help prevent shin splints. Regular warm-up routines and avoiding hard surfaces also reduce risk.
Proper Footwear and Orthotics
Choosing the right footwear is crucial for preventing shin splints. Shoes with adequate arch support, cushioning, and proper fit can reduce stress on the lower legs. Orthotics or shoe inserts may help correct gait issues, such as flat feet or overpronation, which often contribute to shin pain. Wearing shoes designed for your specific activity and replacing them regularly can further minimize the risk of developing shin splints. Proper footwear aligns with effective stretches to promote overall lower leg health.
Warm-Up and Cool-Down Routines
A proper warm-up and cool-down are essential for preventing shin splints. Start with light cardio, such as jogging or cycling, followed by dynamic stretches like leg swings and calf raises. After exercise, cool down with static stretches targeting the calves and hamstrings. Incorporate foam rolling to reduce muscle tension. These routines improve blood flow, reduce muscle stiffness, and minimize the risk of strain on the shins, making them a crucial part of any exercise regimen.
Training Modifications to Avoid Overuse
To prevent shin splints, modify your training by reducing intensity and volume. Alternate hard training days with rest or low-impact activities like swimming or cycling. Gradually increase mileage and intensity to avoid sudden overuse. Incorporate strength and flexibility exercises, such as calf raises and stretches, to support the lower legs. Replace high-impact workouts with low-impact alternatives and ensure proper recovery between sessions. These adjustments help reduce strain on the shins and lower the risk of injury.

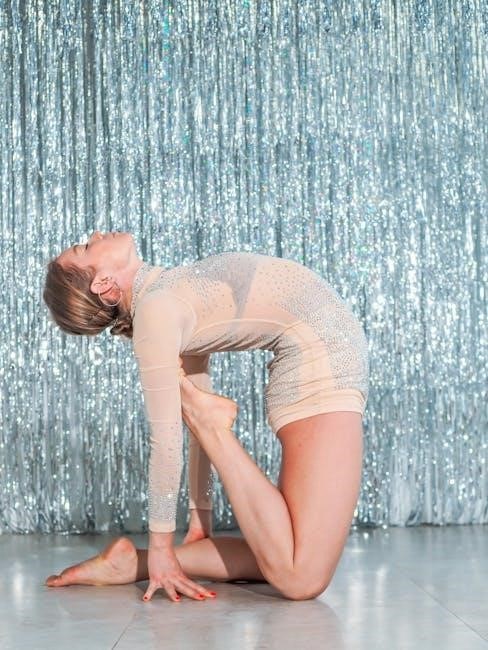
Effective Stretches for Shin Splint Relief
Calf Stretches to Alleviate Tension
Calf stretches help reduce shin splint pain by loosening tight muscles. Stand facing a wall, step one foot back, and gently press the heel down until a stretch is felt.
Calf stretches are essential for relieving shin splint tension. Stand facing a wall, step one foot back, and press the heel down until a stretch is felt. Hold for 20-30 seconds, then switch legs. This targets the gastrocnemius and soleus muscles, reducing tightness that contributes to shin pain. Perform 2-3 sets on each leg. Regular calf stretching improves flexibility and helps prevent future discomfort. Consistency is key for long-term relief and maintaining lower leg health.
Achilles Tendon Stretches for Flexibility
Achilles tendon stretches improve flexibility and reduce tightness that contributes to shin splints. Stand on the edge of a stair with heels hanging off. Slowly lower heels below step level, then rise. Perform 3 sets of 15-20 seconds per leg. This stretch targets the Achilles tendon and calf muscles, promoting relaxation and reducing strain. Regular practice enhances mobility and helps prevent shin-related discomfort. Consistency is key for optimal results and maintaining flexibility.
Shin-Specific Stretches to Reduce Pain
Shin-specific stretches target the tibialis anterior muscle to alleviate pain. Sit on the floor with legs extended. Loop a towel around the ball of one foot and gently pull toward you. Hold for 20-30 seconds, then release. Repeat 3 times per leg. This stretch reduces muscle tension and promotes blood flow to the shin area, helping to relieve discomfort and prevent further strain. Regular practice is essential for maintaining flexibility and managing shin splint symptoms effectively.
Strengthening Exercises to Prevent Recurrence
Strengthening exercises like calf raises, heel drops, and ankle weights target the muscles around the shin, improving endurance and reducing the risk of recurrence effectively.
Toe Raises and Heel Drops
Toe raises and heel drops are essential exercises to strengthen the muscles around the shins, calves, and ankles. Start with toe raises: stand flat, lift toes upward, and hold for 5 seconds. Repeat 15-20 times. Heel drops involve standing on the edge of a stair or platform, lowering heels below the step, and then raising back up. These exercises improve muscle endurance, reduce strain on the shinbone, and help prevent recurrence of shin splints when done consistently.
Ankle Weights and Resistance Bands
Ankle weights and resistance bands are excellent tools for strengthening the lower leg muscles, which can help alleviate shin splint pain. Using ankle weights, perform controlled dorsiflexion and plantar flexion exercises to target the anterior and posterior muscles of the shin. Resistance bands can add extra tension during stretches, improving flexibility and muscle endurance. These exercises should be done gently to avoid further strain, focusing on gradual strength building to support the tibia and surrounding tissues, ultimately reducing shin splint recurrence.
Balance and Stability Training
Balance and stability exercises are crucial for preventing shin splints by improving neuromuscular control and muscle endurance. Single-leg stands, wobble board training, and balance pads can enhance stability around the ankles and shins. These exercises strengthen the smaller stabilizer muscles, reducing the strain on the tibia during physical activities. Start with short durations and gradually increase as balance improves. Proper form is essential to avoid overexertion and maximize the benefits of these exercises for shin health and overall lower leg stability.

Recovery Techniques for Shin Splint Management
Effective recovery involves rest, ice therapy, compression, and elevation to reduce inflammation. Gentle stretching and professional physical therapy can also aid in healing and preventing recurrence.
Ice Therapy and Compression
Ice therapy reduces inflammation by constricting blood vessels, while compression improves blood flow, aiding recovery. Apply ice for 15-20 minutes, 3-4 times daily, using a barrier to prevent skin damage. Compression bandages or sleeves provide support and minimize swelling. Elevate legs above heart level to enhance circulation. Consistency in these techniques accelerates healing and prevents further injury, ensuring a quicker return to physical activities.
Rest and Activity Modification
Rest is crucial to allow the tibia and surrounding muscles to heal. Avoid high-impact activities like running or jumping until pain subsides. Replace with low-impact exercises such as swimming or cycling. Modify training routines by reducing intensity and duration gradually. Incorporate cross-training to avoid overloading the shins. Proper rest and activity modification prevent further injury and promote a faster recovery, ensuring long-term relief from shin splint discomfort.
Physical Therapy and Professional Guidance
Physical therapy plays a vital role in managing shin splints by addressing muscle imbalances and improving flexibility. A licensed therapist can design a personalized program, including targeted stretches and strengthening exercises. Techniques like manual therapy and gait analysis help identify and correct movement patterns contributing to pain. Professional guidance ensures exercises are performed safely and effectively, promoting faster recovery and preventing recurrence. This expertise is especially beneficial for athletes or individuals with persistent symptoms.
When to Seek Professional Help
Consult a healthcare professional if pain persists despite rest, worsens with activity, or is accompanied by swelling, numbness, or difficulty walking, as it may indicate a stress fracture or severe injury.

Recognizing Severe or Persistent Pain
Severe or persistent shin pain that doesn’t improve with rest may indicate a serious issue, such as a stress fracture or chronic inflammation. If the pain worsens during activity, is accompanied by swelling, or limits your ability to walk, it’s crucial to seek medical attention. Persistent pain can lead to long-term damage if untreated. Consult a healthcare professional for proper evaluation and treatment options to avoid further complications and ensure a full recovery.
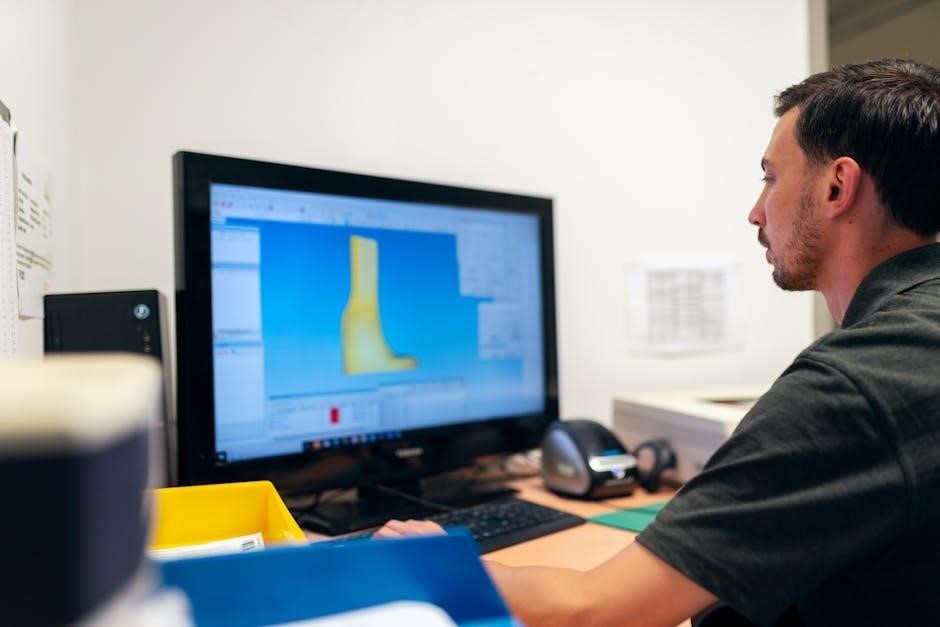
Diagnostic Tests and Medical Evaluation
Medical evaluation for shin splints often includes physical exams, imaging tests like X-rays or MRIs to rule out fractures, and assessing gait mechanics. Professionals may also review activity levels and footwear to identify contributing factors. Proper diagnosis ensures targeted treatment, preventing further injury and promoting recovery. Early evaluation is key to addressing severe cases effectively.
Treatment Options Beyond Home Remedies
Beyond home care, treatments may include physical therapy to strengthen muscles and improve flexibility. Orthotics or shoe inserts can address biomechanical issues, while anti-inflammatory medications reduce swelling. In severe cases, corticosteroid injections or surgery might be recommended. Professional guidance ensures comprehensive recovery and prevents recurrence, offering tailored solutions for lasting relief from shin splint pain and restoring full mobility.

